Understanding and Treating Menstrual Disorders

Menstrual cycles are a natural and fundamental part of a woman’s life, but they can sometimes become a source of pain, discomfort, and disruption. Menstrual disorders are conditions that affect a woman’s normal menstrual cycle, leading to a variety of symptoms ranging from heavy bleeding and severe pain to irregular periods or even the absence of menstruation. These conditions can significantly impact a woman’s quality of life, but with the right diagnosis and treatment, they can be effectively managed. This guide provides a comprehensive overview of common menstrual disorders, their causes, and the various treatment options available.
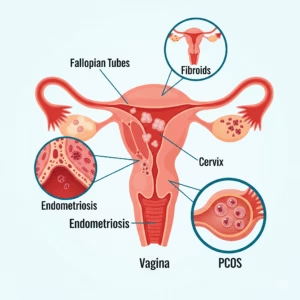
Common Types of Menstrual Disorders
Menstrual disorders can manifest in many different ways. Understanding the specific type of disorder is the first step toward finding an effective treatment.
- Amenorrhea: The absence of menstruation.
- Primary amenorrhea is when a girl has not started her period by age 16.
- Secondary amenorrhea is when a woman who previously had regular periods stops menstruating for three or more consecutive months.
- Dysmenorrhea: Severe and frequent menstrual cramps and pain.
- Primary dysmenorrhea involves pain with no underlying medical condition.
- Secondary dysmenorrhea is caused by a reproductive organ disorder, such as endometriosis or fibroids.
- Menorrhagia: Abnormally heavy or prolonged menstrual bleeding. This can lead to anemia due to significant blood loss.
- Oligomenorrhea: Infrequent or light periods, with cycles lasting longer than 35 days.
- Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD): A combination of physical and emotional symptoms that occur in the week or two before a period. PMDD is a more severe form of PMS.
Causes of Menstrual Disorders
The causes of menstrual disorders are diverse and can range from hormonal imbalances to underlying medical conditions.
| Type of Disorder | Common Causes |
| Amenorrhea | Hormonal imbalances (PCOS, thyroid issues), extreme weight loss or gain, excessive exercise, stress, certain medications. |
| Dysmenorrhea | Uterine fibroids, endometriosis, adenomyosis, pelvic inflammatory disease (PID), ovarian cysts. |
| Menorrhagia | Hormonal imbalances, uterine fibroids or polyps, adenomyosis, IUDs, certain medications, bleeding disorders. |
| Oligomenorrhea | Hormonal changes, stress, eating disorders, PCOS, thyroid issues, perimenopause. |
| PMS/PMDD | Hormonal fluctuations, chemical changes in the brain (serotonin), stress, genetics. |
Understanding these underlying causes is critical for effective treatment. A proper diagnosis from a gynecologist is essential. For women in Gurgaon, a top-rated professional like Dr. Renu Yadav, a gynecologist in Gurugram, can provide expert consultation.
Diagnostic Procedures
To accurately diagnose a menstrual disorder, a doctor will typically perform a thorough physical examination and review your medical history. They may also recommend several diagnostic tests, including:
- Pelvic Exam: A physical examination to check for any abnormalities in the pelvic organs.
- Blood Tests: To check for hormonal imbalances, thyroid problems, or conditions like anemia caused by heavy bleeding.
- Ultrasound: A non-invasive imaging test to visualize the uterus and ovaries and check for conditions like fibroids, polyps, or cysts.
- Hysteroscopy: A procedure where a thin, lighted scope is inserted into the uterus to examine its lining.
- Biopsy: In some cases, a tissue sample from the uterine lining may be taken to rule out serious conditions.
Treatment Options for Menstrual Disorders

The treatment plan for a menstrual disorder depends heavily on the specific condition and its underlying cause. A customized approach is always the most effective.
- Hormonal Therapies:
- Oral Contraceptives (Birth Control Pills): These pills regulate hormone levels, which can help manage irregular periods, reduce menstrual cramps, and lighten heavy bleeding.
- Progesterone Therapy: Can be used to regulate cycles and treat conditions like amenorrhea and oligomenorrhea.
- Hormonal IUD: A device placed in the uterus that releases hormones to reduce heavy bleeding and pain.
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen can effectively reduce pain and inflammation associated with menstrual cramps.
- Tranexamic Acid: A medication that helps reduce heavy bleeding by promoting blood clotting.
- Surgical Procedures:
- Dilation and Curettage (D&C): A procedure to remove the lining of the uterus and reduce heavy bleeding. It is often used for diagnostic purposes as well.
- Hysterectomy: The surgical removal of the uterus. This is a permanent solution for severe cases of menstrual disorders and is typically considered a last resort.
- Myomectomy: A surgical procedure to remove uterine fibroids while preserving the uterus.
- Lifestyle and Home Remedies:
- Diet and Nutrition: Eating a balanced diet rich in iron can help prevent anemia from heavy periods. Limiting caffeine, salt, and sugar can also help reduce PMS symptoms.
- Regular Exercise: Gentle exercise can help alleviate menstrual cramps and improve mood.
- Stress Management: Techniques like yoga, meditation, and deep breathing can help regulate hormones and reduce the impact of stress on the menstrual cycle. According to the World Health Organization (WHO), stress is a significant factor in many health issues, including reproductive health.
- Heating Pad: Applying a heating pad to the abdomen can help relax muscles and ease menstrual cramps.
- Herbal Remedies: Some women find relief from herbal supplements, but it is crucial to consult a doctor before starting any new supplement.
When to See a Doctor
It’s important to know when a menstrual issue requires professional medical attention. You should consult a doctor if you experience:
- Menstrual bleeding that soaks through one or more pads or tampons every hour for several hours.
- Periods that last longer than seven days.
- Severe pain that interferes with daily activities.
- Menstrual cycles that suddenly become irregular after being regular.
- The absence of a period for three or more months.
Seeking timely medical advice from a best gynecologist in Gurgaon, such as Dr. Renu Yadav, can help you get an accurate diagnosis and a personalized treatment plan. Taking care of your menstrual health is an important step toward overall well-being.
Conclusion
Menstrual disorders are common, but they are not something you have to endure. With advancements in medical science, there are numerous effective treatments available to manage symptoms and improve your quality of life. From hormonal therapies and medications to surgical options and lifestyle adjustments, a comprehensive treatment plan can be tailored to your specific needs. If you are experiencing concerning symptoms, do not hesitate to seek professional help. A consultation with a qualified medical expert, like the female gynae doctor Gurgaon trusts, can provide you with the answers and solutions you need. Contact us today to book an appointment with Dr. Renu Yadav and take the first step toward better menstrual health.



